The Power And Perils Of Antibiotics
Let’s get buggy!
Bacteria Basics
Bacteria are single-celled microorganisms. A single staphlococcus bacterium cell is about 1 µm by1µm in size. That’s one-millionth of a meter. (FYI: Viruses are 100 times smaller!)
Bacteria have been on this planet for eons longer than us, and doubtless will persist long after we’re gone. In fact, the earliest bacteria specimens have been found in fossils estimated to be 3.5 billion years old. That makes them the oldest life form on Earth. In fact, the bacteria that causes Lyme disease, Borrelia burgdorferi, may have been around for 15–20 million years, according to fossilized ticks found in amber from the Dominican Republic, although the oldest documented case of Lyme disease is the Tyrolean iceman, a 5,300-year-old mummy found in an Italian Alps glacier.
Nope, they’re not going anywhere.

Caption: Bacteria were some of the earliest life on earth. Some bacteria do leave behind fossils, known as stromatolites (cyanobacteria, blue-green algae)
Your Gut Microbiome
The microbiome of the gut contains approximately 100 trillion bacteria (more than the stars in our galaxy), along with a broad range of viruses and fungi. If you’ve ever needed antibiotics—the medicine that kills off specific, harmful bacteria while also killing off good bacteria—and you’ve gotten an upset stomach and/or diarrhea, or even a yeast infection, you’ve realized just how much you need these helpful little buggers in your system.
Having the right balance of the useful organisms in your gut is essential for health, as they influence how well your body functions:
- Immune system, predisposition towards inflammation and autoimmune illnesses like rheumatoid arthritis and multiple sclerosis, as well as neurological diseases like Parkinson’s and Alzheimer’s disease
- Proper digestion
- Metabolism, weight gain/loss
- Hormones
- Influencing our predisposition towards metabolic syndrome (a precursor of diabetes and heart disease)
- Protection from certain pathogens
- Influence on our cancer risk.
- The wrong type of bacteria can even cause unhealthy aging and affect your mental health. This is why I’ve referred to them as the “psychobiome.”
Your Skin Microbiome
You might not know that your skin also has its own microbiome—over a million bacteria on every square centimeter of skin. It’s like its own ecosystem.
The skin’s microbiome can be ravaged by opportunistic bacteria, such as p. acnes, responsible for the misery of acne. More serious are infections like cellulitis (usually caused by strep or staph infections) or MRSA (Methicillin-resistant Staphylococcus aureus, the “flesh-eating bacteria”), which can be fatal as it is resistant to many of the antibiotics used to treat it.
How Antibiotics Changed the World
Before antibiotics were invented, there were few options to treat bacterial infections: bloodletting, which often killed the patients before the bacteria did; chemical compounds like mercury, arsenic, sulfur, and iodine, which had unpleasant and sometimes lethal side effects; and plant/botanical based medicines, such as quinine, wormwood, and honey. Although natural medicines like Chinese medicine have been around for thousands of years and have been extremely helpful in supporting health–creating the basis of our present pharmaceutical drugs– they have not always been strong enough to control certain bacterial outbreaks. Think Black plague. The epidemic killed up to 50 percent of the European population, where between 75 and 200 million people died in the Middle Ages. We even still have a few cases of the plague today, because the bacteria can live under the ground and in animal reservoirs, but our present antibiotics can control and effectively treat the infection.
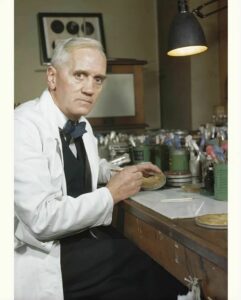
Antibiotics were discovered by accident. Alexander Fleming was a professor of bacteriology at St. Mary’s Hospital in London when he went off on a 2-week vacation in 1928 without realizing he’d made a mistake. Known as a bit of a slob in his lab, he forgot to properly clean up before he left. Thanks to his mess, a culture plate full of Staphylococcus bacteria accidentally got exposed to a mold called Penicillium notatum, and when Fleming examined it upon his return, he realized the bacteria had stopped growing. From there, other scientists were able to develop what became known as penicillin, the first antibiotic.
One of the rare cases where not cleaning up literally changed the world! (I told my wife this story, but unfortunately, it has not changed her view on my role in the after-dinner clean-up).
Penicillin has saved countless millions of lives, especially after it could be used to treat wounded troops during World War II. But now, nearly 100 years later, other mistakes are leaving us far more vulnerable to bacterial infections. Why? Two primary reasons: Antibiotic resistance, and persister cells. These are some of the important keys to effectively treating the Lyme bacteria, Borrelia burgdorferi.
What Is Antibiotic Resistance?
Since antibiotics can only kill certain bacteria, they are completely useless to treat infections caused by anything else, such as viruses or fungi. But because people often insist on getting some kind of treatment from their doctors when they’re sick—and sometimes doctors do think it’s best to take antibiotics as a precaution against secondary infections—antibiotics are sometimes taken when they’re not needed. This oftentimes is the case with a viral upper respiratory infection, when antibiotics are not appropriate. Doing this not only wastes money but can cause debilitating side effects.
It also can lead to antibiotic resistance, where a medication that once worked well is no longer effective. What’s worse is that most animal feed in this country and across the world contains antibiotics. It’s estimated that 40% of antibiotics produced are used as feed additives for animals, and in 2020, the United States used nearly twice as many antibiotics per kilogram of livestock as Europe. The World Health Organization (WHO) and the European health authorities have
attributed this overuse of antibiotics as a major factor contributing to higher levels of antibiotic resistance in some human infections.
Little has been done about the relentless overuse of antibiotics in our food supply. According to a report, “The Role of Antibiotics in Agriculture,” based on an American Academy of Microbiology colloquium in 2001, “The development of antibiotics has provided much success against infectious diseases in animals and humans. But the intensive and extensive use of antibiotics over the years has resulted in the emergence of drug-resistant bacterial pathogens. The existence of a reservoir(s) of antibiotic-resistant bacteria and antibiotic resistance genes in an interactive environment of animals, plants, and humans provides the opportunity for further transfer and dissemination of antibiotic resistance. The emergence of antibiotic-resistant bacteria has created growing concern about its impact on animal and human health.”
Trust me, antibiotic overuse in animals has since gotten much, much worse since 2001. According to a World Health Organization report in 2023, “Antimicrobial resistance (AMR) is one of the top global public health and development threats. It is estimated that bacterial AMR was directly responsible for 1.27 million global deaths in 2019 and contributed to 4.95 million deaths.”


Unless you very carefully vet your meat sources, every time you eat a burger, you’re unwittingly ingesting the same antibiotics fed to the animals on the farms. Not to mention that our habit for significant meat consumption is hurting the planet since these animals are a significant source of methane production; has potential adverse effects on our colon cancer risk and cardiovascular risk, since the breakdown of red meat in the intestine increases levels of a compound known as trimethylamine N-oxide (TMAO) which has been associated with heart disease. All of this while the antibiotics in the meat from animal feed are contributing to your own microbial imbalances and antibiotic resistance. Makes you rethink your diet, doesn’t it?
How and why does antibiotic resistance happen?
It happens not just from overuse and misuse, but is also due to the pesky fact that bacteria are cunning creatures—they haven’t been around for 3.5 billion years without developing characteristics thar keep them going…and going…and going. They continue to mutate and evolve so they won’t die out. And they manage to survive by a mechanism called persister cells and biofilm formation.
What Are Persister Cells?
Persister cells do exactly what they sound like, unfortunately—they persist, which makes them especially dangerous and hard to cure. These microbial cells are a subpopulation of resistant cells that can survive antibiotics or other medications. Often, they hide in biofilms, which are clumps of microbes with cells that stick to each other or on the surface of other cells. They can lay dormant (either non-growing or slow-growing), and can reactivate when conditions are favorable. Certain chronic infections like tuberculosis and leprosy that are slow-growing intracellular infections are persister bacteria and can take up to one year or longer to treat. Persisters not killed by antibiotics can revert to active bacteria in the future when antibiotics are no longer present, and they are in large part responsible for a relapse of the infection.
Persisters have been recognized for other chronic bacterial infections like syphilis (a spirochetal cousin of Lyme disease), as well as bacteria involved in chronic heart valve infections (endocarditis), brucellosis, and Q fever (another tick-borne infection, Coxiella burnetii).
Many persistent infections also involve biofilm formation, such as:
- Gum infections (periodontitis)
- Otitis media (inner ear infections with infections with multiple bacteria, including S. pneumoniae, Hemophilus influenzae, and Moraxella catarrhalis)
- Prosthetic devices (valve and joint replacements)
- Lyme disease.
In 2014, researchers at Johns Hopkins University and Northeastern University showed that Lyme-causing Borrelia was able to form persister bacterial cells. The same process was found for Bartonella, a frequent co-infection I find in my chronically ill Lyme patients. I’ve found that the best way to treat this problem of chronic persistent infections with biofilm/persister forms of the bacteria is with a drug combination that hits the different bacterial forms. These are cell wall forms, cell wall deficient forms (L-forms, S-forms, cystic forms), intracellular forms, and biofilm/persister forms. In the case of Lyme disease, penicillins and cephalosporin antibiotics will effectively hit the growing cell wall forms of the bacteria; antibiotics like metronidazole, tinidazole, hydroxychloroquine, and grapefruit seed extract will address the cystic forms; intracellular antibiotics like tetracyclines and macrolides (azithromycin, for example) will address intracellular forms, but we need specific antibiotics to address these highly resistant biofilm/persister forms. Persister bacteria require 3 and even 4-drug regimens (in the case of resistant TB, even more). Some of the antibiotics used to treat TB, like isoniazid and rifampin, for example, kill growing bacteria, but rifampin and pyrazinamide are also needed to treat active bacteria that arise from reverting persister cells. These antibiotics have changed the course of previously untreatable diseases. We will be devoting a future Substack to the use of persister drugs like dapsone and how/why they’ve made such a difference in changing the course of chronic Lyme disease.
What to Do When You’re Taking Antibiotics
Bottom line: We can’t live without bacteria—but when they’re making us sick, we sometimes can’t live with them at all. Literally. It’s all about balance and homeostasis. Which is why using the 16-point MSIDS model, addressing all the underlying sources of inflammation and their downstream effects is necessary if we are to maintain and support health.
The GI tract is often one source of the inflammation is coming from. It’s also why, if your doctor prescribes an antibiotic (for the right reason), you should remember to take broad spectrum probiotics at least twice a day, first thing in the morning, and last thing at night.
My probiotic regimen:
- I like Theralac from Master Supplements; Orthobiotic from Orthomolecular; saccharomyces boulardii from Xymogen or Orthomolecular, and/or Probiomax 100-350 billion from Xymogen.
- I use these twice a day in my patients while they are on broad spectrum antibiotics, and this regimen is highly effective in keeping down antibiotic associated diarrhea and keeping the GI tract healthy.
- In some cases, I will also use prebiotics, which are fiber supplements that support the growth of healthy bacteria. I like organic flaxseed, chia seed, and hemp seed, and I put these in my low carb yogurt every morning.
- Apart from using the above probiotics, we can also support our microbiome using fiber supplements like Trufiber, from Master Supplements. This gives our bacteria extra nutrition to stay healthy.
- I also like pDC Activate, a postbiotic (Lactococcus lactis strain Plasma), which acts on plasmacytoid dendritic cells (pDC) in the gut. Once activated, pDCs recruit and stimulate nearly all other immune cells, orchestrating a comprehensive immune response by rapidly secreting large quantities of interferons (more than any other immune cell type). Interferons are signaling molecules that trigger the activation and production of various immune cells, including natural killer (NK) cells, B cells and T cells, that each play their own important role in immune defense. By using prebiotics, the right probiotics, and postbiotics, you are providing your body with some of the key elements that are needed for long-term health, especially considering all the bacterial, viral, parasitic, and fungal insults that are now assaulting us on pretty much a daily basis.
Ensuring that you have the right types and balance of bacteria and fungi in your gut is an essential part of staying healthy. I regularly give these probiotics and prebiotics to my patients, where over the past 4 decades, this approach has prevented regular cases of C. difficile diarrhea (a bad bacterial infection that can happen after a round of antibiotics). I also rotate these probiotics every day in my own nutritional supplement protocol even though I am not on antibiotics–the science implicates that the right types of bacteria in our GI tract are intimately involved with our short-term and long-term health. And lately, I added in a postbiotic, to give my immune system another boost. Gut it?
